Hip osteoarthritis (OA, also called degenerative joint disease) is the most prevalent pathologic condition at the hip joint characterised by degeneration of the articular cartilage.
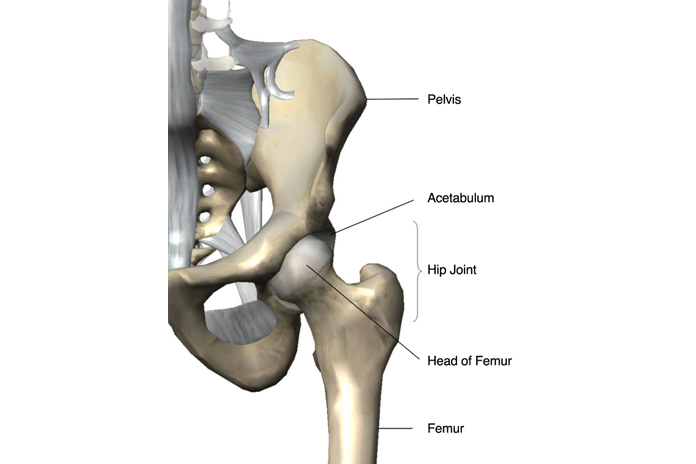
The hip joint (femoro-acetabular joint) is a ball-and-socket type of joint, with the femoral head situated within the concavity formed by the acetabulum and labrum. This anatomic arrangement allows movements in multiple planes, including flexion, extension, adduction, abduction, internal rotation, and external rotation. Significant mechanical forces (three to eight times body weight) are exerted on the hip joint during weightbearing activities such as walking, running, jumping, and lifting. Additional stresses are created by recreational activities (e.g., impacts and falls during sports) and severe trauma (e.g., motor vehicle collisions).
A primary feature of hip OA is cartilage breakdown, thus compromising the femoro-acetabular articulation. In addition the other tissues affected by the disease process include subchondral bone, synovial fluid, ligaments, synovial membrane, joint capsule, and adjacent muscles. Eventually, the joint develops osteophytes (exostosis, marginal bone growth), joint space narrowing, bone sclerosis adjacent to the joint and potentially even joint fusion (arthrosis).
OA can be classified as either primary (idiopathic, unknown cause) or secondary. The most common form of hip OA is primary which is due to ‘wear and tear’ degenerative changes that occur over time. Hip OA is considered secondary if a specific underlying cause can be identified, such as significant prior hip trauma, joint infection or pre existing congenital deformities. Hip trauma is usually significantly associated with unilateral OA, whereas obesity is associated with bilateral OA. Occupational heavy lifting and frequent stair climbing seem to increase the risk of hip OA.
Groin pain is the classic symptom for hip OA. Other symptoms include hip pain, stiffness and associated functional limitations. There can be groin pain with some referred pain down toward the medial knee. Hip OA usually has an insidious onset, is worse with activity particularly with weight bearing and rotational loading of the joint and eases with rest. Advanced OA may be painful even at rest.
Patients with hip OA often have functional limitations in weight bearing activities such as walking, running and climbing stairs. The hip mobility/range of motion restrictions may cause difficulties with activities such as donning or doffing of socks and shoes, picking up clothing from floor and getting in and out of cars. Hip pain and weakness may necessitate use of upper limbs to arise from chair.
Exercise:
An exercise program that includes range of motion, strengthening and aerobic conditioning by walking and aquatic therapy is usually recommended. Strengthening exercises should address all planes of hip movement. Usually the patients may begin with static strengthening exercises to minimize joint movements that could increase the OA symptoms and then progress to dynamic exercises that can maximise strength and function.
Stretching:
This can address mobility/range of motion restrictions in patients with hip OA. Flexibility programs often begin with patients gently moving their joints through the available range of motion (to maintain available range of motion/mobility) and then progress to regaining of lost mobility/range of motion.
Use of Adaptive Equipment:
Hip OA pain may be decreased by using a cane in the opposite hand to the side of OA; this shifts the centre of gravity medially, away from the involved hip thus decreasing the pressure on the hip joint. A shoe lift can correct leg length discrepancy caused by hip joint space narrowing or superior migration of the femoral head within the acetabulum. Adaptive equipment like reachers, sock donners, long-handles shoe horns, elastic shoe laces may help maximize independence despite persistent physical impairments.
Surgery:
Surgery is usually considered in advanced stage of hip OA where there is severe pain and mobility restriction. Surgical treatment of hip OA includes joint realignment joint fusion (arthrodesis) and most commonly joint replacement (arthroplasty). Hip joint arthroplasty Can be categorised as either hemiarthroplasty (prosthetic replacement of the proximal femur while the acetabulum is left intact) or total hip arthroplasty (also called as total hip replacement, with surgical replacement of both the acetabulum and the proximal femur).
Strengthening and Mobility exercises play an important aspect in the treatment of hip OA; the Bambach Saddle Seat can provide the same benefits as the above treatments and can decrease the need for surgical intervention. If exercises are undertaken along with the use of Bambach Saddle Seat, the benefits can be doubled.
The Bambach saddle seat can provide the following benefits
Call 020 8532 5100 (or email ask@fortunabambach.com) and ask for a FREE assessment and demonstration plus 30 day trial. See how effective the Bambach Saddle Seat can be.
References
Cailliet R (2004) Functional Anatomy of the Musculoskeletal System 1st ed. American Medical Association Press, U.S.A
Frontera WR, Silver JK and Rizzo TD (2008) Essentials of Physical Medicine and Rehabilitation 2nd ed. Saunders Elsevier, Philadelphia
Frontera WR and Silver JK (2002) Essentials of Physical Medicine and Rehabilitation 1st ed. Hanley & Belfus, Inc., Philadelphia